CC
PIP Spotlight: Improving Patient Wait Times For New Consults to Pain Management

ABPMR diplomates J.P. McCallin III, MD, and Jason Reed, DO, submitted this Practice Improvement Project (PIP) after noticing long wait times in an outpatient clinic meant new consults to Pain Management faced reduced access to care and were less satisfied with the care they received. Drs. McCallin and Reed led the project with the San Antonio Uniformed Services Health Education Consortium (SAUSHEC) Pain Medicine Fellowship with the goal of improving clinic efficiency and patient satisfaction.
The team identified different causes in the clinic that were leading to longer wait times for patients. Their goal was to decrease the average check-in to roomed and ready for provider time by 15 percent within nine months. After nine months, the team had reduced patient wait time by 27 percent— well over their original goal!
Thank you for sharing your PIP, Dr. McCallin, Dr. Reed, and the SAUSHEC Pain Medicine Fellowship!
The PIP Spotlight is a periodic feature on News Center to highlight exemplary Practice Improvement Projects submitted by your fellow diplomates (or residents) for maintenance of certification (MOC) Part IV credit. Diplomates can use the PIP Spotlight as a tool to plan their own PIPs or as a way to connect with other diplomates doing similar work.
Disclaimer: The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Brooke Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, the Department of the Air Force and Department of Defense or the U.S. Government.

What is the problem you are trying to solve?
There was a clinic inefficiency with regard to the wait time for new patients from check-in to room time to provider evaluation. The wait times in an outpatient clinic reduced the patient's access to care and decreased their overall satisfaction with the care they received.
What data (objective measurements) do you have that supports this as a problem?
Multiple providers were noticing a significant delay in patient evaluation delays from the time of patient check-in. This data was tracked on all new patients for one week to determine if a true problem existed. A total of 51 new patient appointments were included in the sampling. The data revealed:
Average Delays (minutes)
-
Appointment time to check-in: 6.2
-
Check-in to paperwork complete: 16.0
-
Paperwork complete to patient in room: 6.6
-
Patient in room to provider has chart: 5.6
Total Patient Delay: 29.0
What is your opportunity statement? State the goal you hope to achieve.
For new consults to Pain Management, the goal was to decrease the average check-in to roomed and ready for provider time by 15 percent within nine months.
What is the underlying cause of the performance/quality problem?
Numerous meetings with all involved parties— including physicians, physician assistants, med techs, rad techs, LVNs and RNs— were conducted, and we identified these potential problems:
- Patients were waiting in line twice: first to get the check-in paperwork and second to return the completed paperwork
- The amount of paperwork was creating time delays
- There was inefficiency entering data into the electronic medical record (EMR) and scanning the paperwork into the EMR
- Poor communication existed between the front office staff to the medics when the patient was ready to be brought back to a clinic room
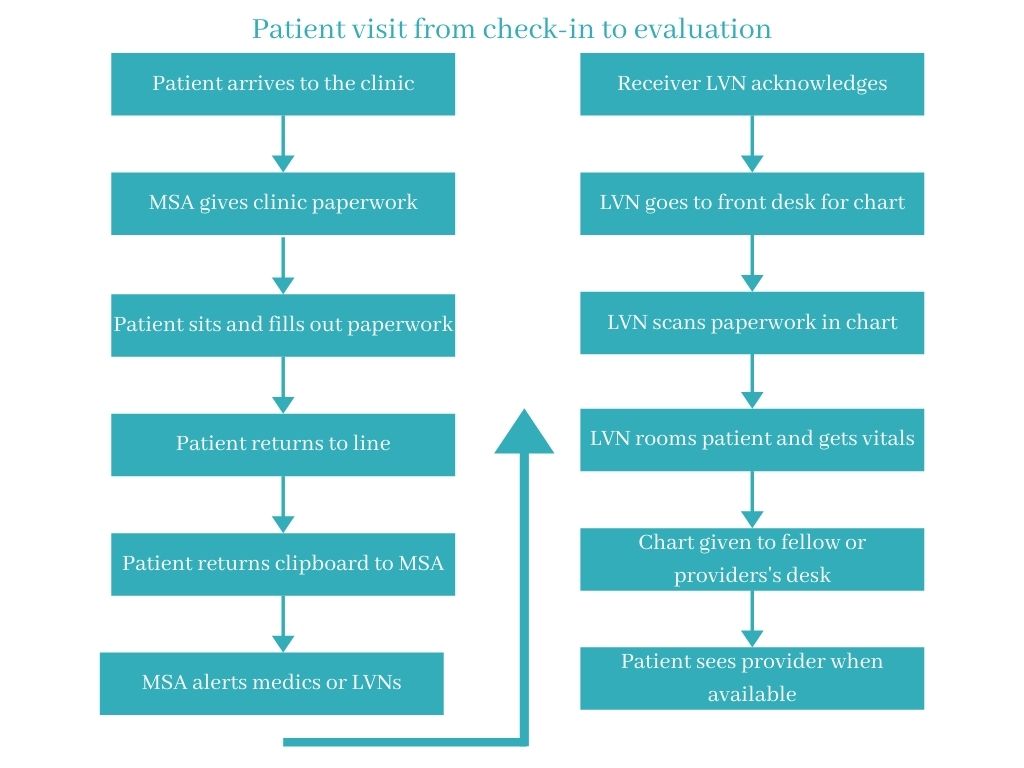
The flowchart below illustrates the process and potential delays a patient experiences from check-in to receiving care.

What change(s) did you implement?
- Eliminated five papers from the check-in folders
- Gave the patient the pain score sheet upon their check-in
- Medic sees that patient checked in on AHLTA (Current EMR), then immediately gets the patient and takes them to a screening room
- Patient's information (including personal information, HPI, PMHx, PSHx, medication reconciliation) is entered into the system by the medic using "hot keys/shortcuts" created for the current EMR to improve efficiency
- When the patient is moved to an examination room, the provider is contacted via clinic voice notification system that the patient is ready
- Provider reviews the information in the AHLTA note that has just been entered then goes to evaluate the patient

Did you achieve your goal or target from your opportunity statement? What data do you have to support your conclusion?
Our goal to decrease patient wait times was met with a 27 percent reduction in room/provider evaluation time— well over the original goal of a 15 percent reduction.
The format utilized for the initial data collection was also used to determine the success/failure of the project with the following results:
Average Delays (minutes)
- Appointment time to check-in: -19.3
- Check-in to room: 7.3
- Patient in room to paperwork complete: 13.0
- Paperwork complete to provider notified: 0.9
Total Patient Delay: 21.1

Will you continue with the changes you have implemented?
Yes. As the medics become more proficient in the screening process, this should continue to improve efficiency for patient wait times. Furthermore, for the first patient on each provider's schedule, the provider evaluation and screening room can be the same room. This will allow the pre-assigned screening rooms to be available for the next patient. We will continue to track the results on a quarterly or bi-annual basis and make changes as necessary.