CC
QI Spotlight: Measuring Muscle Loss in Stroke Survivors with Spasticity

The September QI Project Spotlight was submitted by Sheng Li, MD, PhD.
Dr. Li is Professor in the Department of Physical Medicine and Rehabilitation at McGovern Medical School. His primary clinical focus is spasticity management and neurorehabilitation, mainly after stroke and traumatic brain injury. Dr. Li is the Director of Neurorehabilitation Research Laboratory at TIRR Memorial Hermann Research Center.
Dr. Li focused his QI project on improving DXA (dual-energy X-ray absorptiometry) measurements for post-stroke patients in his rehabilitation hospital. DXA scans were also used to assess the effect BoNT (botulinum toxin) injections had on muscle loss in these patients.
To complete his project, Dr. Li and his team tested possible errors and made changes to the DXA measurement process to improve the quality of DXA scans for their patients.
Thank you for submitting your QI project, Dr. Li!
The QI Project Spotlight (formerly the PIP Spotlight) is a periodic feature on the ABPMR News Center to highlight exemplary Quality Improvement projects submitted by your fellow diplomates (or residents) for continuing certification (CC) credit. Diplomates can use the QI Project Spotlight as a tool to plan their own QIs or as a way to connect with other diplomates doing similar work.

What is the problem you are trying to solve?
I focused on the quality of dual-energy X-ray absorptiometry (DXA) measurements. I practice in a free-standing rehabilitation hospital where our imaging department has a DXA machine. Radiology technicians perform DXA scans and interpret the results provided by the software.
DXA scans measure bone mineral density and soft tissue density, including lean muscles (Figure 1). Data showed there were possible errors in DXA measurements. I worked with the director of our imaging department to investigate the possible underlying causes with the goal to improve the quality and accuracy of DXA measurements.
The primary goals of this project were to assess muscle loss (sarcopenia) in stroke survivors with spasticity, and to investigate the possible effect of botulinum toxin (BoNT) injections on muscle loss in these stroke survivors. The BoNT effect involved repeated DXA scans of the same person before and 2 months after BoNT. The pre- and post-BoNT DXA measures were very confusing, as I detail below.
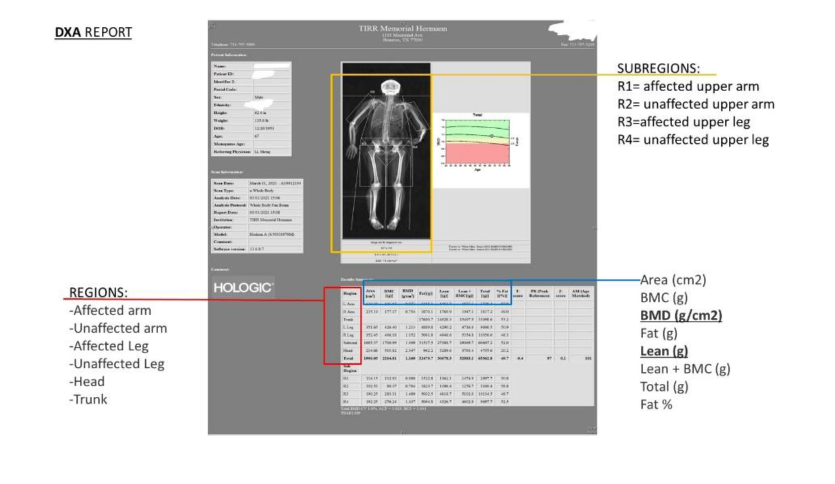
Figure 1: Example of DXA report which provides BMD and lean muscle of the whole body and individual limbs.
What data (objective measurements) do you have that supports this as a problem?
During the initial data collection period (3/1/2021-6/17/2021), we collected DXA results pre- and 2-month post-BoNT injection from five stroke patients with spastic hemiplegia. The results were confusing to the investigative team and the imaging director, as shown in the following examples from two patients.
Both patients received BoNT injections to their affected arm and leg muscles. In Patient 1, there was a 10.9 percent increase in lean muscles in the affected arm, and a 0.8 percent increase in lean muscles in the affected leg. In Patient 2, there was an 18.3 percent decrease in lean muscles in the affected arm, and a 15.7 percent decrease in lean muscles in the affected leg.
In addition to these obvious contrasting results, there was a 36.1 percent decrease in bone mineral density (BMD) and a 43.6 percent increase in lean muscles in the head of Patient 2. This patient did not receive any BoNT injections to the head muscles. In particular, the change in head BMD is simply too large to be true. All these results suggest that there could be errors in DXA measurements.
I asked my research team to stop further data collection for pre- and post-BoNT DXA comparisons after reviewing these contrasting results. I discussed the results with the imaging department director who also expressed concerns. We agreed to investigate the possible underlying cause of this problem.
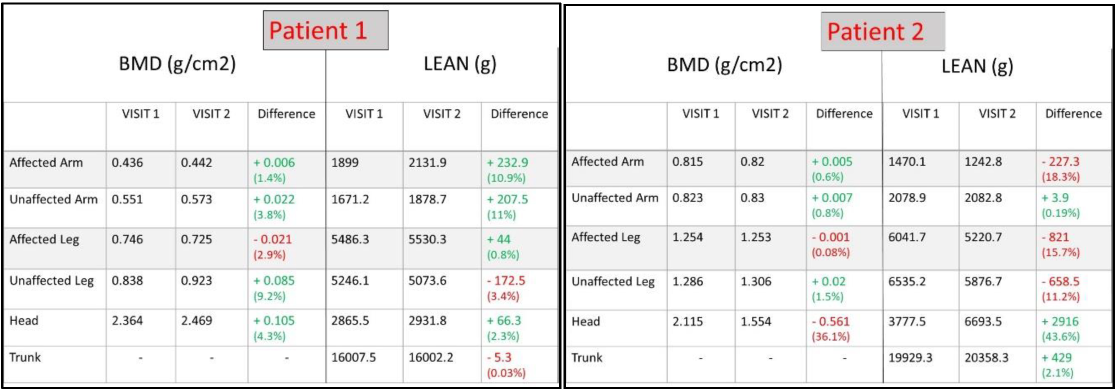
Figure 2: DXA reports of Patient 1 and 2.
What is your opportunity statement? State the goal you hope to achieve.
The ultimate goal is to provide reliable DXA measurements through standardized procedures.
What is the underlying cause of the performance/quality problem?
There are two possible causes: The system error and the operation error. To test the system error, we used a phantom item for system calibration. Briefly, four DXA scans were performed with 10 minute-intervals while keeping the phantom object still on the scan table. As seen in Figure 3, the difference between any two scans was between 0.02 to 1.4 percent. These reports provided us enough confidence that the system itself can generate reliable results.
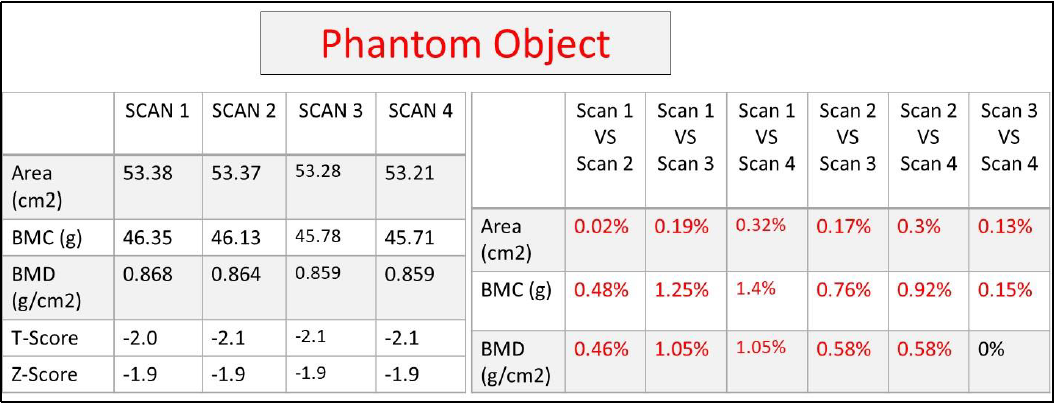
Figure 3: DXA report of a phantom object.
To test the possible operation errors, a healthy volunteer was tested twice with 10 minutes apart. The volunteer was asked to get off the table and return to the table after a short walk outside the test room. We purposefully changed the arm and head positions of the volunteer during the second scan. As shown in Figure 4, decreases in lean muscles for both arms and the head were quite large (from 8.2 percent to 25 percent). These results confirmed that positioning and configuration of the body are important to generate reliable DXA measures.
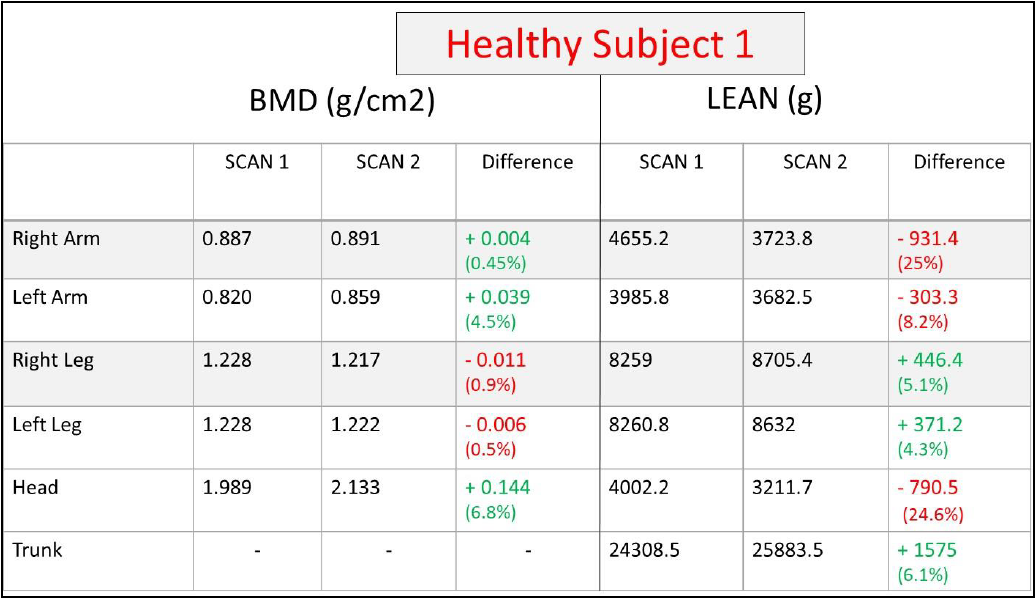
Figure 4: DXA report of a volunteer with different arm position and head orientation.

What change(s) did you implement?
DXA results from repeated scans of a still phantom body and of a healthy volunteer with changing body position provide objective data that show the DXA machine is able to produce reliable results, and changes in body positioning can lead to measurement errors. A standardized operation process is necessary to produce reliable DXA results for patients. After a long discussion with the imaging department director, he agreed that the department needs to make the following changes moving forward:
- Establish a standardized body configuration when a patient is on the scan table
- Train two technicians that are dedicated to DXA scans.
It took two weeks to implement these changes.

Did you achieve your goal or target from your opportunity statement? What data do you have to support your conclusion?
Yes. The DXA results were more reliable after these changes. Another healthy volunteer was tested twice independently by two technicians to check whether we achieve our goal. Technician 1 positioned the volunteer on the scan table in a standardized body configuration. After about 10 minutes, Technician 2 performed another DXA scan on the volunteer. Only the performing technician was in the scan room during each procedure. As shown on Figure 5, the difference between the two independent scans was between -2.6 percent to +2.3 percent.
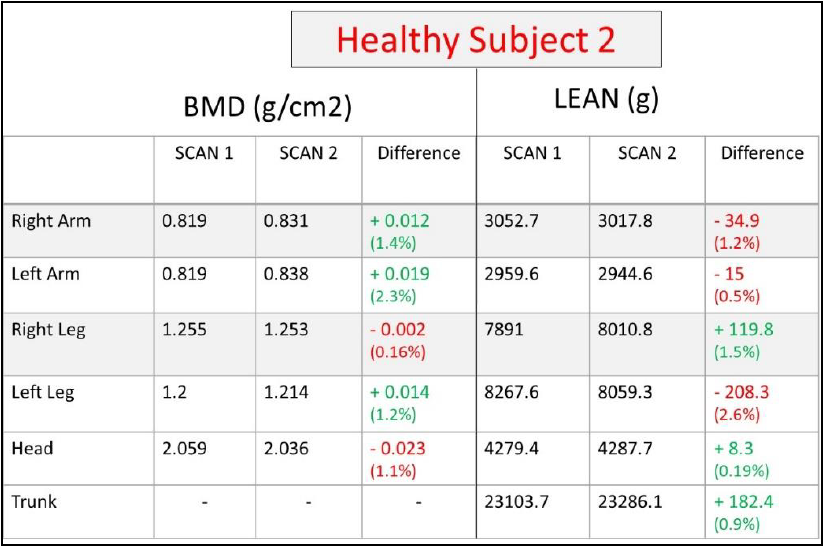
Figure 5: DXA report of a secondary volunteer by two independent technicians.

Will you continue with the changes you have implemented?
Yes. Overall, the implementation of a standardized body positioning and training of two dedicated technicians has significantly improved the quality of DXA measurements. The imaging department director was also convinced that it is necessary to continue these changes, and it is important to keep these changes in order to provide quality DXA measurements for our patients. We plan to resume data collection for pre- and post-BoNT DXA comparisons.

